Supplemental hormones are sometimes effective in reducing or eliminating the pain of endometriosis. The rise and fall of hormones during the menstrual cycle causes endometrial implants to thicken, break down and bleed. Hormone medication may slow endometrial tissue growth and prevent new implants of endometrial tissue.
Hormone therapy isn't a permanent fix for endometriosis. You could experience a return of your symptoms after stopping treatment.
Therapies used to treat endometriosis include:
Hormonal contraceptives. Birth control pills, patches and vaginal rings help control the hormones responsible for the buildup of endometrial tissue each month. Many have lighter and shorter menstrual flow when they're using a hormonal contraceptive. Using hormonal contraceptives — especially continuous-cycle regimens — may reduce or eliminate pain in some cases.
Gonadotropin-releasing hormone (Gn-RH) agonists and antagonists. These drugs block the production of ovarian-stimulating hormones, lowering estrogen levels and preventing menstruation. This causes endometrial tissue to shrink. Because these drugs create an artificial menopause, taking a low dose of estrogen or progestin along with Gn-RH agonists and antagonists may decrease menopausal side effects, such as hot flashes, vaginal dryness and bone loss. Menstrual periods and the ability to get pregnant return when you stop taking the medication.
Progestin therapy. A variety of progestin therapies, including an intrauterine device with levonorgestrel (Mirena, Skyla), contraceptive implant (Nexplanon), contraceptive injection (Depo-Provera) or progestin pill (Camila), can halt menstrual periods and the growth of endometrial implants, which may relieve endometriosis signs and symptoms.
Aromatase inhibitors. Aromatase inhibitors are a class of medicines that reduce the amount of estrogen in your body. Your doctor may recommend an aromatase inhibitor along with a progestin or combination hormonal contraceptive to treat endometriosis.
Conservative surgery
If you have endometriosis and are trying to become pregnant, surgery to remove the endometriosis implants while preserving your uterus and ovaries (conservative surgery) may increase your chances of success. If you have severe pain from endometriosis, you may also benefit from surgery — however, endometriosis and pain may return.
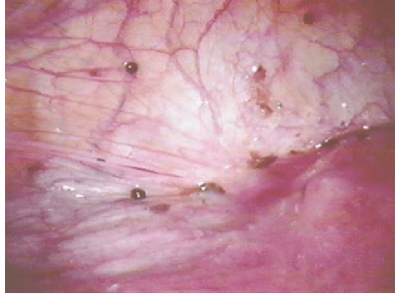
Your doctor may do this procedure laparoscopically or, less commonly, through traditional abdominal surgery in more-extensive cases. Even in severe cases of endometriosis, most can be treated with laparoscopic surgery.
In laparoscopic surgery, your surgeon inserts a slender viewing instrument (laparoscope) through a small incision near your navel and inserts instruments to remove endometrial tissue through another small incision. After surgery, your doctor may recommend taking hormone medication to help improve pain.
Fertility treatment
Endometriosis can lead to trouble conceiving. If you're having difficulty getting pregnant, your doctor may recommend fertility treatment supervised by a fertility specialist. Fertility treatment ranges from stimulating your ovaries to make more eggs to in vitro fertilization. Which treatment is right for you depends on your personal situation.
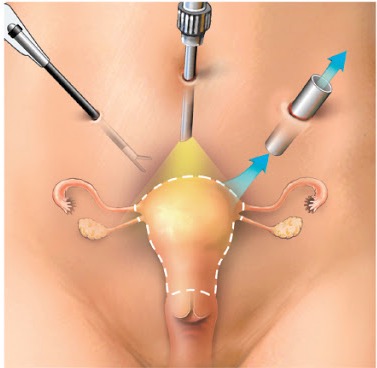
Hysterectomy with removal of the ovaries
Surgery to remove the uterus (hysterectomy) and ovaries (oophorectomy) was once considered the most effective treatment for endometriosis. But endometriosis experts are moving away from this approach, instead focusing on the careful and thorough removal of all endometriosis tissue.
Having your ovaries removed results in menopause. The lack of hormones produced by the ovaries may improve endometriosis pain for some, but for others, endometriosis that remains after surgery continues to cause symptoms. Early menopause also carries a risk of heart and blood vessel (cardiovascular) diseases, certain metabolic conditions and early death.
Removal of the uterus (hysterectomy) can sometimes be used to treat signs and symptoms associated with endometriosis, such as heavy menstrual bleeding and painful menses due to uterine cramping, in those who don't want to become pregnant. Even when the ovaries are left in place, a hysterectomy may still have a long- term effect on your health, especially if you have the surgery before age 35.
Finding a doctor with whom you feel comfortable is crucial in managing and treating endometriosis. You may want to get a second opinion before starting any treatment to be sure you know all of your options and the possible outcomes.
What you can do
Your first appointment will likely be with either your primary care physician or a gynecologist. If you're seeking treatment for infertility, you may be referred to a doctor who specializes in reproductive hormones and optimizing fertility (reproductive endocrinologist).
- Make a list of any symptoms you're experiencing. Include all of your symptoms, even if you don't think they're related.
- Make a list of any medications, herbs or vitamin supplements you take. Include how often you take them and the doses.
- Have a family member or close friend accompany you, if possible. You may get a lot of information at your visit, and it can be difficult to remember everything.
- Take a notepad or electronic device with you. Use it to make notes of important information during your visit.
- Prepare a list of questions to ask your doctor. List your most important questions first, to be sure you address those points.
If you, or someone you care about, has endometriosis, it is important to research the disease as much as possible. Many myths and misconceptions about endometriosis still persist, even in the medical literature. Endometriosis can be a challenging condition to manage. An early diagnosis, a multidisciplinary medical team and an understanding of your diagnosis may result in better management of your symptoms and improving quality of life.